01 May Falls Prevention
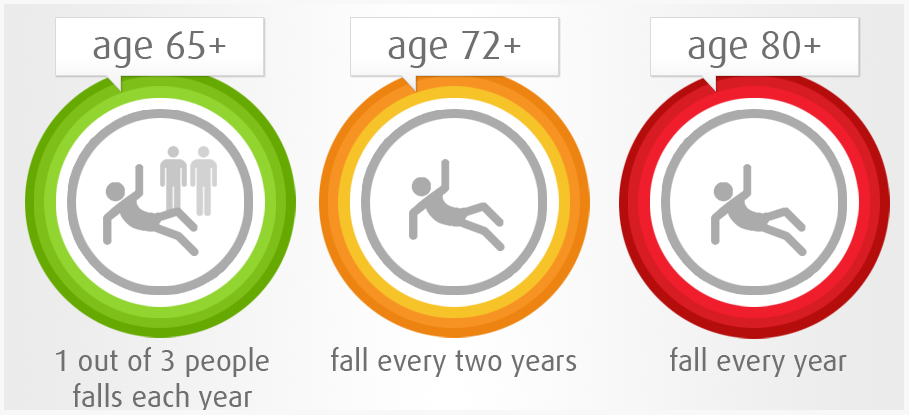
In New Zealand 30-60% of those aged over 65 fall, and off those up to 20% result in injury, hospitalisation, or death. By 2035 the number of those over the age of 65 will have doubled resulting in 500000 falls costing up to $100 million in medical costs, not including the vast social cost.
Falls happen due to a change / deterioration in the combination of 3 key components. 1. Physiological function 2. The environment and 3. Behavior
To avoid falling, a sighted ambulant person needs adequate vision to observe environmental challenges (eg, uneven or slippery surfaces); proprioception (awareness of where body parts are in space); reaction time to respond to unexpected movements; and sufficient muscle strength to correct against the forces of gravity
Natural aging, muscle disuse, medication and disease can all disrupt how these systems function and coordinate together. There can also be specific risk factors, such as cataracts affecting vision, that need to be addressed individually on top of the general program.
Multiple studies show programs are successful, with up to a 42% reduction in falls with programs that are done frequently (2 hours a week for 6 months). For success they must include balance work.
A good exercise program is based on four premises:
- The program needs to be individually tailored because older people vary considerably in their physical capacity and health and in their response to exercise. This also takes into account the individual risk factors mentioned above.
- The program will need to be increased in difficulty, because there will be improvements in strength and balance over time.
- It should be a sustainable program that can continue to be done. It is recommended that it should be checked every 2-3 months for compliance and to be updated.
- A walking program to increase physical capacity can complement the strength and balance program
Outlined below are the important components to make a program successful.
Exercise must provide a moderate or high challenge to balance. Exercises should aim to challenge balance in three ways:
- Reducing the base of support (e.g. standing with both legs close together, standing with one foot directly in front of the other, i.e. a tandem stance position and, if possible, standing on one leg).
- Movement of the centre of gravity – control of the body’s position while standing (e.g. reaching safely, transferring the body weight from one leg to the other, stepping up onto a block).
- Reducing the need for upper limb support with exercises in standing that do not use the arms for support.
Exercise must be of a sufficient dose to have an effect. Therefore it is recommended that exercise should be undertaken for at least 2 hours per week.
- Ongoing exercise is necessary. Gains are lost if you stop doing exercise.
- Falls prevention exercise programs benefit all older people.
- Falls prevention exercise can be used in both a group or a home-based setting.
- Though walking programs are not needed, walking training may be included in addition to balance training.
- Strength training is a valuable addition to balance training
For further advice talk to one of the physiotherapists here at The Lakes Clinic.


Sorry, the comment form is closed at this time.